Interventional ultrasound refers to diagnostic or therapeutic minimally-invasive procedures guided by real-time ultrasound imaging. Examples of this are needle insertions for the extraction of tissue (biopsy), for the delivery of cancer-treating seeds (brachytherapy), and for the delivery of anesthesia for pain relief of labour (epidural).
As part of a NSERC/CIHR grant on epidural anesthesia, we developed a new ultrasound scanning protocol for guiding epidural needle insertions. Such insertions are used for pain relief of women in labour, but the failure rate of such insertions is 6-20%. Possible complications of epidurals include headaches, nerve damage, paralysis and death. This is a very challenging procedure where competency of 80% is reached only after 60 attempts on patients. Together with Dr. Kamani at BC Women’s Hospital, we have developed specialized ultrasound imaging technology to replace the current blind needle insertions in order to reduce complications and increase the learning curve. Since anesthesiologists currently rely only upon their sense of feel to indicate where the needle tip is inserted relative to the spinal cord, we have also introduced novel computer-based instrumentation to quantify this sense of feel. A clinical study performed at BC Women’s Hospital in 2007 showed that pre-puncture ultrasound could provide guidance of the depth of the epidural space from the skin surface with an accuracy of a few mm – sufficient for guidance. This study also included the instrumentation of the sense of feel. This research was awarded 2nd place for oral presentations at the 36th Annual UBC Department of Anesthesiology, Pharmacology and Therapeutics Research Competition and Awards Night. The extension of this work for different needle trajectories was awarded 1st place for poster presentations the following year. A second clinical trial was performed at BC Women’s Hospital in 2008 where ultrasound was performed before and during needle insertion. In that study, all patients were successfully guided by ultrasound, including patients with obesity and scoliosis – traditionally very difficult patients. The impact of the second trial is large because it empowers anesthesiologists to perform ultrasound guidance in the operating room while watching live on the monitor the needle advance towards the target. This study will have far-reaching implications because it puts the ultrasound directly in the hands of the operator performing the needle insertion. This work was presented at the 2008 annual meeting of the Society for Obstetric Anesthesia and Perinatology (SOAP) where it was nominated for the Zuspan competition for best paper. A new grant was awarded in 2009 to further this research on thoracic epidural insertions for surgery.
We have developed a series of groupwise ultrasound to CT registration algorithms for guiding percutaneous needle-based spinal interventions. These registration schemes use a biomechanical model that accounts for changes in the curvature of the spine between preoperative and intraoperative imaging. In our intensity-based registration methodology, each vertebra in CT is treated as a sub-volume and transformed individually. The biomechanical model is used to constrain the displacement of the vertebrae relative to one another. The sub-volumes are then reconstructed into a single volume. During each iteration of registration, an US image is simulated from the reconstructed CT volume and an intensity-based similarity metric with the real US image is calculated. We have also developed a feature-based registration technique. For further information, please refer to Gill et al. and Rasoulian et al.
NEW – A website has been created to highlight the opportunities and challenges of ultrasound scanning the lumbar spine for epidural guidance: www.epiduralultrasound.com.
Ultrasound-gu
ided Orthopaedic Surgery
We have developed a series of ultrasound-guided orthopaedic surgery applications. One example is an application developed for the management of scaphoid bone fractures. The scaphoid bone is the most frequently fractured bone in the wrist, representing about 90% of all wrist fractures. In general, the bone is fractured through its relatively narrow waist. Due to poor blood supply, complications are common. In case of complications, internal fixation of the scaphoid is often the only remaining treatment option. Percutaneous fixation reduces many of the drawbacks associated with an open approach. The traditional percutaneous procedure, however, requires many harmful, intra-operative fluoroscopic images to ensure an accurate screw placement. The 2D nature of fluoroscopic images limits the 3D positioning of surgical tools. Furthermore, the small bones in the wrist joint overlap each other in lateral fluoroscopic images.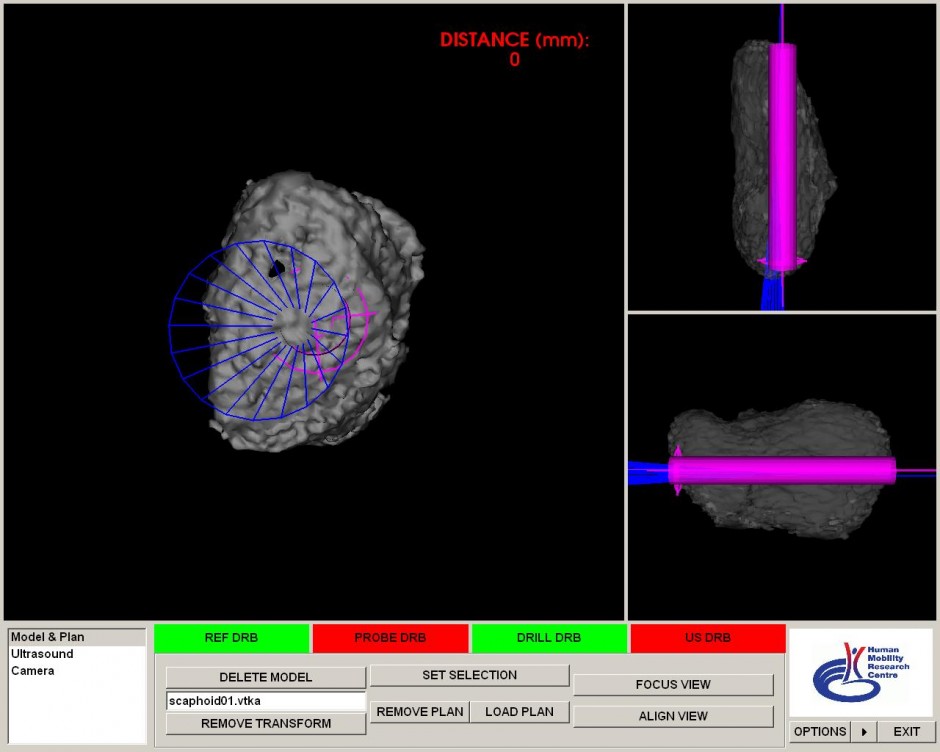
We have developed a new surgical navigation system for percutaneous scaphoid fixation. The system uses harmless ultrasound imaging for intra-operative registration of a pre-surgery plan to the patient in the operating room. Laboratory experiments proved that the accuracy and consistency of the new approach are significantly improved with respect to conventional fluoroscopic percutaneous fixation. For further information, please refer to Beek et al.
Another example is an ultrasound-guided shoulder arthroscopy technique. For further information, please refer to Tyryshkin et al.
